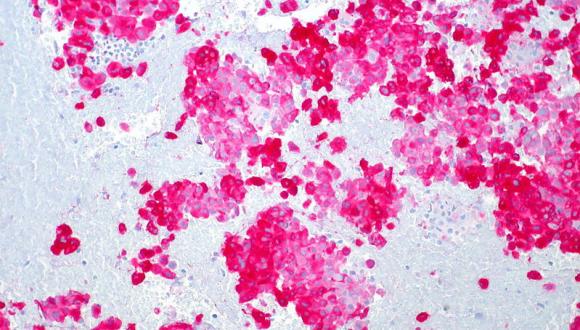
TAU Scientists Honored for Cutting-Edge Proposals in Melanoma Research
Melanoma is the deadliest form of skin cancer. For their cross-disciplinary melanoma research proposals, two teams of TAU scientists and doctors received a total of $1.35 million. Leading the teams are Prof. Ronit Satchi-Fainaro of TAU's Sackler Faculty of Medicine's Department of Physiology and Pharmacology and head of TAU's Cancer Angiogenesis and Nanomedicine Laboratory; and Dr. Gal Markel, of TAU's Sackler Faculty of Medicine's Department of Microbiology and Clinical Immunology and head of the research laboratory at TAU's Ella Institute for the Treatment and Research of Melanoma and Skin Cancer at Sheba Medical Center.
How cancer cells move to the brain
Prof. Satchi-Fainaro and her colleagues — Dr. Neta Erez of the Sackler Faculty's Department of Pathology, and Prof. Zvi Ram, head of the Department of Neurosurgery at Tel Aviv Medical Center — received $900,000 for a proposal that explores how melanoma cells form metastases in distant organs, especially the brain. Prof. Satchi-Fainaro and her multidisciplinary team are working to identify the precise pro-metastatic factors secreted from astrocytes, special brain cells, which may constitute "druggable targets" for future nanotherapies.
"The whole field of nanomedicines for cancer is based on the fact that nanometric-size drugs (around 10-200 nanometers) are too large to leak out from normal blood vessels and harm healthy organs," said Prof. Satchi-Fainaro. "On the other hand, tumor blood vessels are incredibly leaky, so the nanomedicines can selectively exit from those blood vessels and accumulate at the tumor mass. Once at the tumor site, the new nanomedicines can inhibit the cross-talk between the melanoma cells and the brain microenvironment. We hope that our novel approach for co-targeting melanoma cells and astrocytes will pave the road for new clinical interventions."
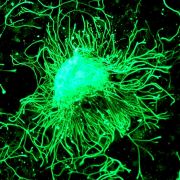
A disarmament proposal for tumor cells
The MRA granted its second Team Science Award of $450,000 to Dr. Gal Markel and his team — Dr. Tamar Geiger of TAU's Sackler Faculty of Medicine's Department of Human Molecular Genetics and Biochemistry, and Dr. Noam Shomron, director of TAU's Sackler Faculty of Medicine's Functional Genomics Laboratory. The focus of their study is to discover the mechanisms that allow tumors to evade the immune system, then to disarm those mechanisms, making the tumor susceptible to the patient's own immune response.
"Immunotherapy, which has existed for decades, has had slim success rates in melanoma treatment. But now, after new insights and developments over the last 10 years, it has become a hot topic everyone is discussing," said Dr. Markel. "We are focused on the immunology of melanoma — how the immune system reacts to melanoma cells, how melanoma evades the immune system, and defining key processes."
Dr. Markel's team is working directly with melanoma patients who are treated with immunotherapy. "We are taking advantage of our years of unique clinical work, bringing it to the bench for a cutting-edge multi-faceted discovery process," Dr. Markel says.
To date, the MRA, which is the largest private funder of melanoma research, has awarded more than $51 million worldwide to advance prevention, diagnosis, and treatment. Based in Washington, DC, the alliance's ultimate goal is to find a cure by funding the most promising melanoma research worldwide that will accelerate progress and improve outcomes for patients and all who are at risk.
As originally reported by AFTAU