New study reveals critical insights in fight against skin cancer

Research
New study reveals critical insights in fight against skin cancer

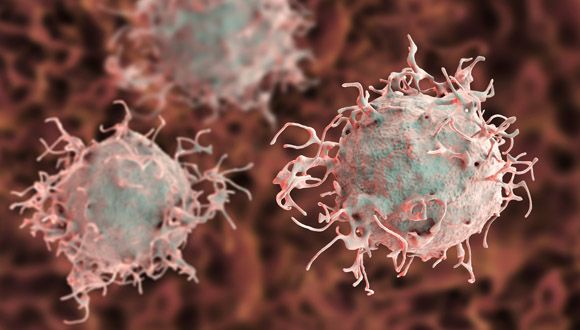
A new study conducted at Tel Aviv University and the Sheba Medical Center reveals how melanoma cancer cells affect their close environment to support their needs - by forming new lymph vessels in the dermis to go deeper into the skin and spread through the body. The researchers believe that the new discovery may contribute to the development of a vaccine against the deadly cancer.
The scientific breakthrough was led by Prof. Carmit Levy of Tel Aviv University's Sackler Faculty of Medicine and Prof. Shoshana Greenberger from the Sheba Medical Center. The study was funded by ICRF (the Israel Cancer Research Fund) and its results appeared in the Journal of Investigative Dermatology published by Nature.
"We demonstrated for the first time that in the first stage, in the epidermis, melanoma cells secrete extracellular vesiculas called melanosomes." - Prof. Shoshana Greenberger

The researchers (from left): Prof. Carmit Levy and Prof. Shoshana Greenberger
Melanoma, the deadliest of all skin tumors, starts with uncontrolled division of melanocyte cells in the epidermis – the top layer of the skin. In the second stage the cancer cells penetrate the dermis and metastasize through the lymphatic and blood systems.
In previous studies a dramatic rise was observed in the density of lymph vessels in the skin around the melanoma - a mechanism that was not understood by researchers until now.
"Our main research question was how melanoma impacts the formation of lymph vessels, through which it then metastasizes," explains Prof. Greenberger. "We demonstrated for the first time that in the first stage, in the epidermis, melanoma cells secrete extracellular vesiculas called melanosomes."
What are these vesiculas and how do they impact their environment? Examining this in human melanomas from the Pathology Institute, the researchers demonstrated that melanosomes could penetrate lymph vessels. They then examined their behavior in the environment of actual lymph vessel cells and found that here too the melanosomes penetrate the cells and give them a signal to replicate and migrate. In other words, the primary melanoma secretes extracellular vesiculas that penetrate lymph vessels and encourage the formation of more lymph vessels near the tumor, enabling the melanoma to advance to the lethal stage of metastasis.
"If we can stop the mechanisms that generate metastases in lymph nodes, we can also stop the disease from spreading" - Prof. Shoshana Greenberger
Prof. Carmit Levy adds that, "melanoma cells secrete the extracellular vesiculas, termed melanosomes, before cancer cells reach the dermis layer of the skin. These vesicles modify the dermis environment to favor cancer cells. Therefore, melanoma cells are responsible for enriching the dermis with lymph vessels, thereby preparing the substrate for their own metastasis. We have several continuing studies underway, demonstrating that the melanosomes don't stop at the lymph cells, as they also impact the immune system, for example."
Since melanoma is not dangerous at the premetastatic stage, understanding the mechanism by which the metastases spread via the lymphatic and blood systems can hopefully contribute to the development of a vaccine against this deadly cancer.
"Melanoma that remains on the skin is not dangerous," says Prof. Greenberger. "Therefore, the most promising direction for fighting melanoma is immunotherapy: developing a vaccine that will arouse the immune system to combat the melanosomes, and specifically to attack the lymphatic endothelial cells already invaded by the melanosomes. If we can stop the mechanisms that generate metastases in lymph nodes, we can also stop the disease from spreading."

Research
CPAT, a groundbreaking Tel Aviv University development, offers promising results with sustained improvement months after treatment

Attention Deficit Hyperactivity disorder (ADHD) is one of the most common mental disorders affecting children. Symptoms of ADHD include inattention, hyperactivity, and impulsivity, and the disorder is considered a chronic and debilitating disorder that affects many aspects of an individual's life, including academic and professional achievements, interpersonal relationships, and daily functioning.
Tel Aviv University has developed a new treatment called Computerized Progressive Attention Training (CPAT), which has shown remarkable efficacy in alleviating symptoms of Attention Deficit Hyperactivity Disorder (ADHD) among students. In fact, a notable 33% of students experienced significant improvements in their symptoms when undergoing CPAT, surpassing the improvement in symptoms of only 11% of the students who participated in a parallel protocol involving mindfulness training. During this mindfulness training, students practiced a specific form of meditation designed to mitigate their attention difficulties. Importantly, the benefits of CPAT also outshone those of drug treatments like Ritalin, as the improvements persisted for up to four months after the completion of the treatment protocol.
The study was the doctoral dissertation of Dr. Pnina Stern, under the guidance of Prof. Lilach Shalev-Mevorach of The Jaime and Joan Constantiner School of Education at Tel Aviv University. The encouraging results of the study were recently accepted for publication in the Journal of Attention Disorders.
“We developed the CPAT system years ago, and it produced good results in previous studies that we conducted, mainly in children," explains Prof. Shalev-Mevorach. "Furthermore, in the only study that we conducted in adults with ADHD, positive findings were obtained, but without indications of ‘far transfer,’ meaning an improvement in functions for which participants were not directly trained in the treatment.”
According to Prof. Shalev-Mevorach, it is challenging for researchers to make scientific claims about the effectiveness of non-medication treatments because it is difficult to compare them to a "non-medication placebo." In other words, when studying non-medication treatments, it's hard to distinguish the effects of the treatment itself from other factors like the attention participants receive during training sessions or the effort they put into the research. This makes it complex to determine the true impact of non-medication interventions.

Prof. Lilach Shalev-Mevorach
In the current study, the team of researchers tried to resolve this by employing a research design that included two control groups: a regular control group, which performed the various assessment tasks at two points in time without any intervention as part of the research (the passive control group) and a second control group that participated in mindfulness training sessions under the guidance of a professional instructor. This type of training has yielded positive results in previous studies in people with ADHD.
For the experiment 54 students, male and female, diagnosed with ADHD were recruited from Tel Aviv University and other academic institutions. The subjects were blindly divided into three groups: a zero-intervention control group, a mindfulness group and a CPAT group.
Participants in the CPAT and the Mindfulness groups attended two-hour long group meetings on the University campus once a week, where the CPAT group received Computerized Progressive Attention Training and the mindfulness group received training from a certified mindfulness instructor.
Before and after the intervention protocol, the participants of the three groups performed a comprehensive series of assessment tests: standard computerized tests to assess attention functions, behavioral assessment questionnaires (self-reported ADHD symptoms), and mindfulness questionnaires (self-reported feelings such as stress, anxiety and well-being). In addition, a novel measurement was used for this intervention study, whose participants were, as mentioned, higher-education students: they were asked to read a text from a scientific article while their eye movements were tracked by an eye-tracker. The indices produced using the eye-tracking system made it possible to identify a pattern of inattentive reading, which was used as a measure of reading efficiency in an academic context. Finally, the participants filled out a questionnaire regarding their academic difficulties.
Prof. Shalev-Mevorach says the results were very positive: “We saw improvements in the attention functions themselves, that is, ‘near transfer,’ for example in sustained attention, the ability to remain attentive for a long period of time, and in attention control, the ability to delay a routine response. But the main thing, is that we saw significant improvements in the participants’ daily and academic functioning, such as reduced repeated reading while reading a scientific article. Furthermore, the improvements in these attention functions were connected to the reduction in behavioral symptoms of ADHD and in repetitive reading."
"In other words, the CPAT trained the attention mechanisms themselves, and their improvement was related to the improvement achieved in behavioral symptoms and reading patterns. 33% of the participants who received the CPAT protocol showed a significant improvement in ADHD symptoms, compared to only 11% of those who underwent the mindfulness protocol. The improvements obtained were preserved in the testing that was carried out about four months after the end of the intervention protocol.”
Prof. Shalev-Mevorach notes that the effects of stimulant drugs (psychostimulants) such as Ritalin and Concerta are ‘on-off’: patients who take Ritalin daily enjoy significant improvements, but when they stop the treatment, the improvements fade, and they return to the starting point. She says the researchers wish to bring about "a profound change in basic attention functions, a change that will be significant in the long term, as an additional option alongside medication, and of course as an alternative to drug treatment in cases in which it isn’t applicable.”

Research
The role of hope in supporting mental health

The role of hope in supporting mental health is not sufficiently understood among relevant professionals, according to Dr. Dorit Redlich Amirav of TAU’s Department of Occupational Therapy, Steyer School of Health Professions, Sackler Faculty of Medicine.
“Hope is similar to the air we breathe,” says Redlich Amirav. “Air is taken for granted in our daily life until we are suffocating and struggling to breathe.”
Redlich Amirav studies how different groups implement hopeful thinking and improve mental well-being through meaningful occupations. Through her findings, she aspires to help mental health professionals to integrate concepts of hope into their research and treatment and, in the long run, provide a longer-lasting and greater impact on each patient’s holistic well-being.
"Hope is similar to the air we breathe. Air is taken for granted in our daily life until we are suffocating and struggling to breathe." - Dr. Dorit Redlich Amirav
In new research published in Qualitative Health Research, she investigated the cross-generational transmission of hope. Redlich Amirav cites one of her female participants who was forced by her grandfather to quit school in sixth grade. She felt her hope diminish but stated that her hopeless personal circumstances led her to put more of an emphasis on the importance of education and studying with her own two daughters who both graduated from university.
Other participants displayed this particular kind of cross-generational hope. For example, a mother told Redlich Amirav about her father, who was a violinist until the Nazis broke his fingers. The mother internalized this trauma in a negative way, but all four of her own children play instruments and one of them is an opera singer. She inadvertently conveyed how hope and music are intertwined for them and their heritage.
In 2019, Redlich Amirav was appointed director of the Israeli chapter of the International Hope Barometer. She says that it came just in time: hope became a key factor in successfully adapting to the trials and tribulations of the pandemic. During the lockdowns, she says that people found meaning in new ways of interacting; specific trends point to the importance of goal-directed behavior in increasing hope.
Source: TAU Review

Research
New study reveals that brain's coordination between hippocampus and cortex during sleep boosts memory consolidation, offering hope for people with memory impairments

While a good night's sleep is known to be critical for the consolidation of long-lasting memories, so far there has been little evidence regarding the precise processes at work during human sleep. A breakthrough study demonstrated for the first time that long-lasting memories are consolidated in the human brain through communication between the hippocampus and the cerebral cortex during sleep. Moreover, the researchers found that by inducing deep-brain stimulation during sleep they can improve memory consolidation. They believe intervention during sleep represents a unique approach that can be further developed in the future to provide hope for people with memory impairments such as dementia.
The unique study, which was published in the leading journal Nature Neuroscience, involved an international collaboration led by Dr. Maya Geva-Sagiv (today at UC Davis). The study was a collaboration between the laboratories of Prof. Yuval Nir from the Sackler Faculty of Medicine, Department of Biomedical Engineering at The Iby and Aladar Fleischman Faculty of Engineering, and Sagol School of Neuroscience at Tel Aviv University, and Prof. Itzhak Fried from the Department of Neurosurgery at UCLA and the Sackler Faculty of Medicine at Tel Aviv University.
"Intervention during sleep represents a unique approach that can be further developed in the future to provide hope for people with memory impairments such as dementia." - Prof. Yuval Nir

The researchers (from left to right): Dr. Maya Geva-Sagiv, Prof. Yuval Nir and Prof. Itzhak Fried
"This study was made possible by a rare group of 18 patients with epilepsy at the UCLA Medical Center," says Prof. Nir. "Prof. Fried implanted electrodes in these patients' brains to try and pinpoint the areas that cause their epileptic seizures, and they volunteered to take part in a study investigating the effects of deep-brain stimulation during sleep. Close work with expert neurologists led by Prof. Dawn Eliashiv at UCLA enabled our team to integrate advanced brain stimulation in the research. Thus, we were able to test, for the first time in humans, the long-held hypothesis - that coordinated activity of the hippocampus and cerebral cortex during sleep is a critical mechanism in consolidating memories."
"Moreover, we improved memory consolidation through a special stimulation protocol that enhanced synchronization between these two areas in the brain. Intervention during sleep represents a unique approach that can be further developed in the future to provide hope for people with memory impairments such as dementia."
"In this study we directly examined the role of neural activity and electrical brain waves during sleep. Our goal was to enhance the natural mechanisms at play, to discover exactly how sleep assists in stabilizing memories." – Dr. Maya Geva-Sagiv
"We know that a good night's sleep is critical for the consolidation of long-lasting memories, but so far, we had little evidence regarding the precise processes that are at work during human sleep," explains Dr. Maya Geva-Sagiv. "In this study we directly examined the role of neural activity and electrical brain waves during sleep. Our goal was to enhance the natural mechanisms at play, to discover exactly how sleep assists in stabilizing memories."
The researchers developed a deep-brain stimulation system that improves electrical communication between the hippocampus – a deep-brain region involved in acquiring new memories, and the frontal cortex – where memories are stored for the long term. By monitoring activity in the hippocampus during sleep, the system enables precisely timed delivery of electrical stimulation to the frontal cortex.
The study's participants completed two memory tests, and their performance was compared after two different nights – one undisturbed and one with deep-brain stimulation. On both occasions, they were asked in the morning to recognize famous persons whose pictures they had been shown the previous evening. The study found that deep-brain stimulation significantly improved the accuracy of their memory.
"To our surprise, we also discovered that the intervention did not significantly increase the number of right answers given by participants, but rather reduced the number of wrong answers. This suggests that sleep sharpens the accuracy of our memory…" - Prof. Yuval Nir
"We found that our method had a beneficial effect on both brain activity during sleep and memory performance," says Prof. Fried. "All patients who had received synchronized stimuli to the frontal cortex demonstrated better memory performance, compared to nights of undisturbed sleep. The control group, which received similar yet unsynchronized stimuli, showed no memory improvement. Our deep-brain stimulation method is unique because it is close-looped – stimuli are precisely synchronized with hippocampal activity. In addition, we monitored the stimuli's impact on brain activity at a resolution of individual neurons."
"Our findings support the hypothesis that precise coordination between sleep waves assists communication between the hippocampus that takes in new memories, and the frontal cortex that stores them for the long term," adds Prof. Nir.
"To our surprise, we also discovered that the intervention did not significantly increase the number of right answers given by participants, but rather reduced the number of wrong answers. This suggests that sleep sharpens the accuracy of our memory, or in other words, it removes various distractions from the relevant memory trace."
The study was supported by grants from the US National Institutes of Health (NIH), the European Research Council (ERC), the US National Science Foundation (NSF), the US-Israel Bilateral Science Foundation (BSF), and the Human Frontier Science Program (HFSP). The paper’s other co-authors are: Prof. Dawn Eliashiv, Dr. Emily Mankin, Natalie Cherry, Guldamla Kalender, and Dr. Natalia Tchemondanov of UCLA, and Dr. Shdema Epstein from Tel Aviv University.