A breakthrough method delivers two drugs straight to the cancer site.
Research
A breakthrough method delivers two drugs straight to the cancer site.
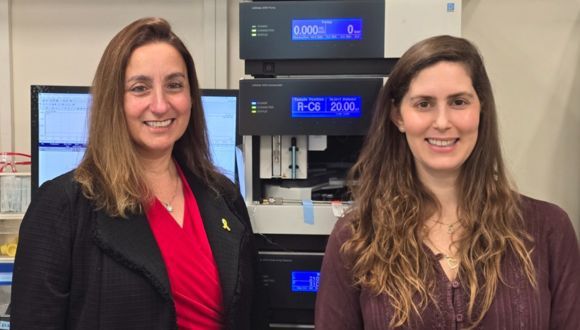
Researchers at Tel Aviv University have developed a new platform using polymeric nanoparticles to deliver drug pairs to specific cancer types, including skin and breast cancer. The researchers explain that having both drugs arrive at the tumor site significantly amplifies their therapeutic effects and safety profiles.
The study was led by Prof. Ronit Satchi-Fainaro and doctoral student Shani Koshrovski-Michael from the Department of Physiology and Pharmacology at Tel Aviv University's School of Medicine, in collaboration with other members of Prof. Satchi-Fainaro's lab: Daniel Rodriguez Ajamil, Dr. Pradip Dey, Ron Kleiner, Dr. Yana Epshtein, Dr. Marina Green Buzhor, Rami Khoury, Dr. Sabina Pozzi, Gal Shenbach-Koltin, Dr. Eilam Yeini, and Dr. Rachel Blau. They were joined by Prof. Iris Barshack from the Department of Pathology at Tel Aviv University's School of Medicine, Prof. Roey Amir and Shahar Tevet from the School of Chemistry at Tel Aviv University, and researchers from the Israel Institute of Biological Research, Italy, Portugal, and the Netherlands. The study was published in the prestigious journal Science Advances.
Bringing Precision to Drug Partnerships
Prof. Satchi-Fainaro explains: "Currently, cancer treatment often involves a combination of multiple drugs that work synergistically to enhance their anti-cancer effect. However, these drugs differ in their chemical and physical properties – such as their rate of degradation, their circulation time in the bloodstream, and their ability to penetrate and accumulate in the tumor. Therefore, even if multiple drugs are administered simultaneously, they don't arrive together at the tumor, and their combined effects are not fully realized. To ensure maximal efficacy and minimal toxicity, we sought a way to deliver two drugs simultaneously and selectively to the tumor site without harming healthy organs".
The researchers developed biodegradable polymeric nanoparticles (which break down into water and carbon dioxide within one month) capable of encapsulating two different drugs that enhance each other's activity. These nanoparticles are selectively guided to the cancer site by attaching them to sulfate groups that bind to P-selectin, a protein expressed at high levels in cancer cells as well as on new blood vessels formed by cancer cells to supply them with nutrients and oxygen.
The researchers loaded the platform with two pairs of drugs approved by the FDA: BRAF and MEK inhibitors used to treat melanoma (skin cancer) with a BRAF gene mutation (present in 50% of melanoma cases), and PARP and PD-L1 inhibitors intended for breast cancer with a BRCA gene mutation or deficiency. The novel drug delivery system was tested in two environments: in 3D cancer cell models in the lab and in animal models representing both primary tumor types (melanoma and breast cancer) and their brain metastases.
The findings showed that the nanoparticles, targeted toward P-selectin, accumulated selectively in primary tumors and did not harm healthy tissues. Furthermore, the nanoparticles successfully penetrated the blood-brain barrier, reaching metastases in the brain with precision without harming healthy brain tissue.
Additionally, the combination of two drugs delivered simultaneously was far more effective than administering the drugs separately, even at 30 times lower doses than prior preclinical studies. The nanoparticle treatment significantly reduced tumor size, prolonging time to progression by 2.5 times than standard treatments, and extended the lifespan of mice treated with the nanoparticle platform. Mice had a 2-fold higher median survival compared to those receiving the free drugs and a 3-fold longer survival compared to the untreated control group.
A New Approach to Cancer Treatment
Prof. Satchi-Fainaro summarized: "In our study, we developed an innovative platform using biodegradable polymeric nanoparticles to deliver pairs of drugs to primary tumors and metastases. We found that drug pairs delivered this way significantly enhanced their therapeutic effect in BRAF-mutated skin cancers and BRCA-mutated breast cancers and their brain metastases. Since our platform is versatile by design, it can transport many different drug pairs that enhance each other’s effects, thereby improving treatment for a variety of primary tumors and metastases expressing the P-selectin protein, such as glioblastoma (brain cancer), pancreatic ductal adenocarcinoma, and renal cell carcinoma".
The project received competitive research grants from Fundación “La Caixa”, the Melanoma Research Alliance (MRA), the Israel Science Foundation (ISF), and the Israel Cancer Research Fund (ICRF). It is also part of a broader research effort in Prof. Satchi-Fainaro’s lab supported by an Advanced Grant from the European Research Council (ERC), ERC Proof of Concept (PoC), EU Innovative Training Networks (ITN), and the Kahn Foundation.

Research
This breakthrough could pave the way for neurological treatments.
Researchers at Tel Aviv University have developed an innovative research model that allowed them to decode the mechanism underlying a severe and rare neurological disease. The disease is characterized by symptoms such as epilepsy, developmental delay, and intellectual disability.
According to the researchers: "Decoding the disease mechanism is a critical step toward developing treatments targeting specific cellular functions for this disease and other conditions with similar mechanisms affecting cellular energy production".
The research was led by Tel Aviv University’s Prof. Abdussalam Azem, Dean of the Wise Faculty of Life Sciences, in collaboration with Prof. Uri Ashery and PhD student Eyal Paz from the School of Neurobiology, Biochemistry and Biophysics at the Wise Faculty of Life Sciences and the Sagol School of Neuroscience. Additional contributors included Dr. Sahil Jain and Dr. Irit Gottfried from the School of Neurobiology, Biochemistry, and Biophysics at Tel Aviv University, Dr. Orna Staretz-Chacham from the Faculty of Health Sciences at Ben-Gurion University, Dr. Muhammad Mahajnah from the Technion, and researchers from Emory University in Atlanta, USA. The findings were published in the prominent journal eLife.
Prof. Azem explains: "The disease we studied is caused by a mutation in a protein called TIMM50, which plays a crucial role in importing other proteins into the mitochondria—the organelle considered the cell's energy powerhouse. The human mitochondria operate with about 1,500 proteins (approximately 10% of all human proteins), but only about 13 of them are produced within the mitochondria itself. The rest are imported externally through various mechanisms. In recent years, mutations in the TIMM50 protein, which is responsible for importing about 800 proteins into the mitochondria, were found to cause severe and rare neurological disease with symptoms like epilepsy, developmental delay, and intellectual disability".
Prof. Ashery adds: "Protein import into the mitochondria has been extensively studied over the years, but how a mutation in TIMM50 affects brain cells was never tested before. To investigate this for the first time, we created an innovative model using mouse neurons that mimics the disease caused by the TIMM50 protein mutation. In this study, we significantly reduced the expression of the protein in mouse brain cells and observed its impact on the cells".
Eyal Paz explains: "The impairment of the protein led to two main findings: a reduction in energy production in the neurons, which could explain the developmental issues seen in the disease and an increase in the frequency of action potentials (the electrical signals that transmit information along neurons and enable communication between them). This increase in action potential frequency is known to be associated with epilepsy. The change in frequency is likely caused by significant damage to two proteins that function as potassium channels. Imbalances in potassium levels can lead to life-threatening conditions, such as arrhythmias, cardiac arrest, and muscle weakness, potentially leading to paralysis. These potassium channels may serve as potential targets for future drug treatments for the disease".
Prof. Azem concludes: "Our study decodes the mechanism of a severe and rare neurological disease caused by a mutation in a protein critical for importing proteins into the mitochondria. Understanding the mechanism is a crucial step toward treatment, as it enables the development of drugs targeting the specific issues identified. Additionally, we created a new research model based on mouse neurons that significantly advances the study of protein import into mitochondria in brain cells. We believe that our findings, combined with the innovative model, will enable more in-depth research and the development of treatments for various neurological diseases caused by similar mitochondrial dysfunction mechanisms".