3D Printing Takes on Brain Cancer
Major TAU development enables new and improved treatments for deadly glioblastoma
Tel Aviv University researchers have 3D-printed a first-of-its-kind glioblastoma tumor that mimics a living cancer malignancy, powering new methods to improve treatment and accelerate the development of new drugs for the most lethal type of brain cancer.
Breakthrough in the Battle against Brain Cancer
Glioblastoma is notoriously fatal as it accounts for the majority of brain tumors and is highly aggressive. The average survival time of patients with glioblastoma is 14-15 months from diagnosis. Glioblastoma spreads quickly and in an unpredictable manner, making it particularly challenging to treat with existing approaches including surgery, radiation therapy, chemotherapy and certain targeted therapies. New drugs could drive better patient outcomes. However, existing drug development methods in the lab are time-consuming and don’t show how a treatment will work in an individual patient’s body.
To address the matter, the TAU research team created the world's first fully functioning 3D model of a glioblastoma tumor, which includes 3D-bioprinted cancer tissue and the surrounding tumor environment that affects its development. The findings were published recently in the journal Science Advances.
WATCH: TAU researchers explain their breakthrough development
“Our innovation gives us unprecedented access to 3D tumors that better imitate the clinical scenario, enabling optimal investigation," says the study's lead researcher, Prof. Ronit Satchi-Fainaro of the Sackler Faculty of Medicine, the Sagol School of Neuroscience, and the Director of the Morris Kahn 3D-BioPrinting for Cancer Research Initiative at Tel Aviv University. “Cancer, like all tissues, behaves very differently in a petri dish or test tube than it does in the human body. Approximately 90% of all experimental drugs fail in clinical trials because the success achieved in the lab is not reproduced in patients."
Gateway for Personalized Medicine?
"If we take a sample from a patient's tumor, together with surrounding tissues, we can 3D-bioprint from this sample 100 tiny tumors and test many different drugs in various combinations to discover the optimal treatment for this specific tumor,” she explains. “Alternately, we can test numerous compounds on a 3D-bioprinted tumor and decide which is most promising for further development and investment as a potential drug.”
Satchi-Fainaro, a 2020 Kadar Family Award laureate for her nanoparticle vaccine research studying cancers and COVID-19, adds that perhaps the most exciting aspect of her team’s breakthrough is identifying proteins and genes in cancer cells that can serve as new targets for drugs – a particularly difficult task when dealing with a tumor inside the brain of a living being.
For example, the researchers were able to use their new technology to target a specific protein mechanism they had previously identified that causes the immune system to help glioblastoma spread, rather than attack deadly cancer cells. The experiment succeeded in delaying the growth and blocking the invasion of glioblastoma.
According to Prof. Satchi-Fainaro, this innovative approach will not only enable the discovery of new drug targets, but also enable the development of new drugs at a much faster rate than today. She hopes that in the future, this technology will facilitate personalized medicine for patients.
Launchpad for Advancement
The 3D-bioprinted tumor is made from a gel composition that resembles the brain and includes a complex system of blood vessel-like tubes through which blood cells and drugs can flow, simulating how a real tumor develops and reacts to treatments.
“The process in which we bio-print a tumor from a patient is that we go to the operating suite, we extract tissue from the tumor and we print it according to the MRI of that patient,” explains Satchi-Fainaro, who is also Director of the Cancer Biology Research Center and Head of the Cancer Research and Nanomedicine Laboratory at Tel Aviv University. “Then, we have about two weeks in which we can test all the different therapies to evaluate their efficacy for that specific tumor, and get back with an answer about which treatment is predicted to be the best fit.”
Using biological samples from patients, the researchers teamed up with Dr. Asaf Madi's lab at TAU's Department of Pathology, Sackler Faculty of Medicine, to conduct genetic sequencing of the cancer cells in the 3D model. With their approach, the researchers could replicate the specific growth rate and behavior of each tumor. As a result, Satchi-Fainaro says, "We proved that our 3D-printed model is better suited for predicting treatment efficacy, drug target discovery and new drug development.”

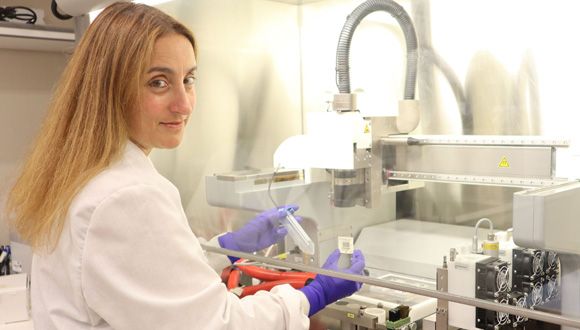
The research team from left: Eilam Yeini, Lena Neufeld and Prof. Satchi-Fainaro (Photo: Tel Aviv University)
The 3D technology was developed by PhD student Lena Neufeld, together with other researchers at Satchi-Fainaro's laboratory: Eilam Yeini, Noa Reisman, Yael Shtilerman, Dr. Dikla Ben-Shushan, Sabina Pozzi, Dr. Galia Tiram, Dr. Anat Eldar-Boock and Dr. Shiran Farber.
The 3D-bioprinted models are based on samples from patients, taken directly from operating rooms at the Neurosurgery Department of the TAU-affiliated Tel Aviv Sourasky Medical Center (Ichilov Hospital).
The study was funded by the Morris Kahn Foundation, European Research Council (ERC), Israel Cancer Research Fund (ICRF), the Israel Cancer Association and Israel Science Foundation (ISF), and Check Point Software Technologies LTD.